CRISPR set on HIV cure
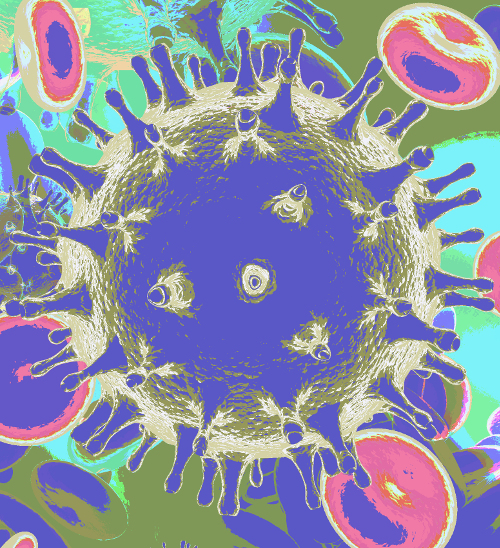 Gene editing technology has been used to test a potential HIV cure.
Gene editing technology has been used to test a potential HIV cure.
A team from the Amsterdam UMC in the Netherlands has used CRISPR-Cas gene editing technology to eliminate HIV from infected cells in a lab environment.
The approach addresses one of the most formidable challenges in HIV treatment: the virus's capacity to embed itself into the human genome, requiring continuous antiviral therapy to prevent resurgence.
The new technique uses CRISPR-Cas technology. Awarded the Nobel Prize in Chemistry in 2020, this technology enables precise modifications to the genomes of living organisms. Acting on guide RNA (gRNA) directives, CRISPR-Cas functions as molecular ‘scissors’ to specifically target and cut HIV DNA integrated into the host's genetic material. The Amsterdam UMC's research centres on a novel strategy employing two gRNAs against conserved sequences within the HIV genome.
These sequences remain constant across various HIV strains, enabling a universal therapy approach capable of addressing multiple variants of the virus.
One significant obstacle encountered by the team was the large size of the vector required to deliver the therapeutic CRISPR-Cas components into cells.
The researchers used some innovative methods to reduce the vector's size, likening the challenge to fitting oversized luggage into a compact car, to ensure efficient delivery to target cells.
The study evaluated different CRISPR-Cas systems derived from bacteria, focusing on their efficacy and safety in treating HIV-infected CD4+ T cells.
The findings revealed that saCas9, one of the systems tested, demonstrated exceptional antiviral capabilities, completely inactivating HIV with a single gRNA and successfully excising viral DNA with two gRNAs.
This strategy not only minimised the vector size but also targeted hidden HIV reservoir cells, particularly those expressing specific surface proteins (CD4+ and CD32a+), where the virus could rebound when antiretroviral therapy is halted.
Despite these encouraging results, the researchers caution that the path to a functional HIV cure is still in its infancy, saying that the current findings serve as a proof of concept rather than an imminent therapeutic solution.
The next steps involve optimising the delivery mechanisms to target a broader range of HIV reservoir cells and combining CRISPR therapeutics with receptor-targeting agents for preclinical model testing.
This approach aims to strike a balance between efficacy and safety, a crucial consideration for advancing towards clinical trials.
Details of the study, led by Dr Elena Herrera-Carrillo, along with team members Yuanling Bao, Zhenghao Yu, and Pascal Kroon, will be presented at the European Congress of Clinical Microbiology and Infectious Diseases (ECCMID 2024) in April.








 Print
Print