Clear chip for blood studies
 Research engineers have developed a ‘blood vessel-on-a-chip’ that could improve diagnostics and reduce the use of animal testing.
Research engineers have developed a ‘blood vessel-on-a-chip’ that could improve diagnostics and reduce the use of animal testing.
Experts say the innovative technology has the potential to revolutionise drug testing and development for heart disease.
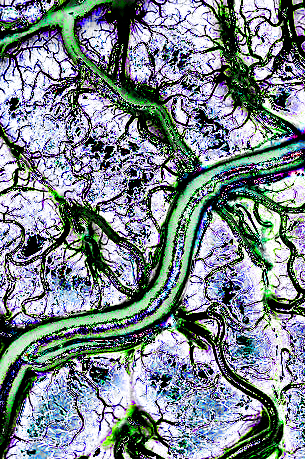
The microchip, which is transparent, mimics the initial stage of heart disease development caused by high blood flow and inflammation.
This design provides a detailed and accurate understanding of how and why blockages occur in specific locations within blood vessels.
“This is an incredible development because we took advantage of these microchips being made from a transparent material, and we mimicked the conditions of the coronary artery, that supplies blood to the heart muscle, and imaged them with a microscope to map the areas of cell damage which were similar to the locations of blockages in patients with heart disease,” says Associate Professor Anna Waterhouse, from the Charles Perkins Centre and the Sydney Nano Institute.
The transparency of the microchip allows for precise imaging of cell damage, a level of detail that is not achievable with traditional animal models.
“If we use an animal model, we are unable to see changes at this level of detail in a living organism because you can’t see through the vessels,” Waterhouse said.
Cardiovascular disease remains the leading cause of mortality globally, responsible for over 18 million deaths each year.
The new technology holds significant promise for improving the understanding and treatment of this widespread health issue.
The development of the ‘blood vessel-on-a-chip’ has been documented in two academic papers published in Advanced Functional Materials and Advanced Materials Technologies.
The device features tiny channels where human cells can grow, mimicking the structure and function of human blood vessels.
This setup enables scientists to conduct tests quickly and efficiently, using minimal liquid and providing results that are more relevant to human biology compared to animal models.
“Innovations like this in the field of organ-on-a-chip technology are crucial for potentially benefiting millions worldwide, offering faster and more cost-effective development of drugs without relying on animal testing,” Waterhouse said.
The researchers aim to use these findings to further explore the potential of the microchip in biomedical applications, particularly in modelling human organs and diseases. This could lead to a better understanding of human biology and more effective drug screening.
“We want to further our research by testing devices that simulate complex interactions within human organs, enabling us to replicate more advanced disease stages, such as severe heart disease or advanced cancer," said Associate Professor Waterhouse.
Future developments include incorporating additional types of vascular cells to better mimic human blood vessels and adding fats to replicate cholesterol build-up, the next stage in heart disease progression.
The team is also working on applying their surface modification technique to sensors and diagnostic tools.








 Print
Print